Unveiling Digital Pathology – Its Evolution, Benefits, And the Future Trends With AI
Digital pathology has become widespread beyond academic labs. It is also crucial in pharmaceutical companies and contract research organizations (CROs). It is rapidly transforming the way pathologists diagnose and conduct research on diseases.
In this article, we will learn about digital pathology, its benefits and evolution, and the relationship between Digital pathology and Artificial intelligence.
What Is Digital Pathology?
Digital pathology is the acquisition, management, sharing, and interpretation of pathology information, such as slide images and data, in a digital format.
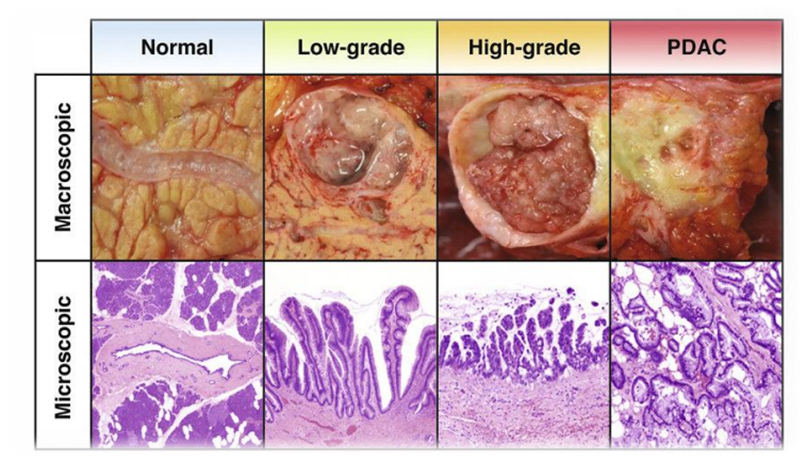
The Glass slides containing tissue samples are scanned using advanced digital scanners to produce high-resolution digital slide images. These images can be easily seen through computer screens and mobile devices, enabling greater accessibility and efficiency.
What Are the Benefits of Digital Pathology?
Digital pathology is quite beneficial from the perspective of patient care. It also plays an essential role in laboratory billing services by submitting accurate CPT Codes for pathology tests.
The top three benefits of digital pathology in healthcare are the following;
- It enables rapid referral of cases across pathology networks, allowing patients to access the best pathologists and top-notch treatments.
- Improves laboratory workflow and connectivity among different labs to increase workforce efficiency.
- Ensures rapid dissemination of information through digital slides and WSI, which helps patients avoid having to undergo the same test again at different localities.
Evolution of Digital Pathology – From Telepathology to Whole Slide Imaging (WSI)
Ever wonder how Digital pathology has evolved? This technique’s evolution started with telepathology, where motorized microscopes were used to transmit live views of slides for consultations.
However, with time, the technique of sharing slides improved, and today, Whole Slide Imaging (WSI) has become the gold standard.
What is Whole Slide Imaging (WSI)?
Whole Slide Imaging (WSI) refers to scanning complete tissue slides and creating a high-resolution image that is easily accessible, either onsite or from another central database.
WSI requires solid infrastructure, such as strong IT systems with components like;
- Image scanners
- Servers
- High-speed data bandwidth.
For remote access, the bandwidth should be at least 10 Mbps for uninterrupted image downloads.
What are Category III CPT codes?
The Category III Current Procedural Terminology (CPT) code is a unique subset used by health professionals, nonphysician practitioners, hospitals, and outpatient facilities to track the utilization of emerging technologies, services, and procedures.
How Are These Codes Useful in Digital Pathology?
These codes are used for;
- Tracking and evaluating new pathology services
- Reporting procedures and services to federal and private payers for reimbursement of rendered healthcare.
- Consider transitioning them to permanent Category I codes with particular reimbursement rates.
In pathology medical billing services, these CPT codes;
- Ensure on-time reimbursement
- Improve Revenue Cycle Management (RCM) for laboratories.
Category III New CPT Codes for Digital pathology
Category III CPT Codes are assigned to emerging technologies, services, and procedures in Digital pathology.
Digital pathology CPT Codes for Blood Smear:
- 0854T: Digitization of glass microscope slides for blood smear analysis.
CPT Code for Bone Marrow:
- 0855T: Digitization of glass microscope slides for bone marrow examination.
CPT Codes for Consultation:
- 0838T: Digitization of glass microscope slides prepared in-house.
- 0839T: Digitization of glass microscope slides prepared elsewhere.
- 0840T: Digitization of glass microscope slides prepared in-house with additional stains.
CPT Codes for Cytopathology:
- 0827T: Digitization of glass microscope slides for cervical/vaginal.
- 0828T: Digitization of glass microscope slides for non-gynecological.
- 0829T: Digitization of glass microscope slides for fine needle aspiration.
- 0830T: Digitization of glass microscope slides for urine.
- 0831T: Digitization of glass microscope slides for cerebrospinal fluid.
- 0832T: Digitization of glass microscope slides for body fluids.
- 0833T: Digitization of glass microscope slides for sputum.
- 0834T: Digitization of glass microscope slides for bronchial washings.
- 0835T: Digitization of glass microscope slides for bronchial brushings.
- 0836T: Digitization of glass microscope slides for gastric washings.
- 0837T: Digitization of glass microscope slides for other sources.
CPT Code for Electron Microscopy:
- 0856T: Digitization of glass microscope slides for electron microscopy.
CPT Code for Immunofluorescence:
- 0845T: Digitization of glass microscope slides for immunofluorescence, direct method.
- 0846T: Digitization of glass microscope slides for immunofluorescence, indirect method.
CPT Code for Immunohistochemistry:
- 0760T: Digitization of glass microscope slides for the first stain.
- 0761T: Digitization of glass microscope slides for each additional stain.
- 0762T: Digitization of glass microscope slides for multiplex stain.
CPT Code for Intraoperative Pathology Consultation:
- 0841T: Digitization of glass microscope slides for intraoperative first tissue block.
- 0842T: Digitization of glass microscope slides for intraoperative each additional tissue block.
- 0843T: Digitization of glass microscope slides for intraoperative frozen section.
- 0844T: Digitization of glass microscope slides for intraoperative touch preparation.
CPT Code for Molecular Analysis:
- 0847T: Digitization of glass microscope slides for molecular analysis.
CPT Code for Morphometric Analysis:
- 0763T: Digitization of glass microscope slides for morphometric analysis.
- 0851T: Digitization of glass microscope slides for morphometric analysis of first tissue block.
- 0852T: Digitization of glass microscope slides for morphometric analysis of each additional tissue block.
- 0853T: Digitization of glass microscope slides for frozen section.
In Situ Hybridization:
- 0848T: Digitization of glass microscope slides for in situ hybridization, first probe.
- 0849T: Digitization of glass microscope slides for in situ hybridization, each additional probe.
- 0850T: Digitization of glass microscope slides for in situ hybridization, multiplex probe.
CPT Code for Special Stain:
- 0756T: Digitization of glass microscope slides for special stain, first stain.
- 0757T: Digitization of glass microscope slides for special stain, each additional stain.
- 0758T: Digitization of glass microscope slides for special stain, multiplex stain.
- 0759T: Digitization of glass microscope slides for special stain, frozen section.
CPT Code for Surgical Pathology:
- 0751T: Digitization of glass microscope slides for surgical pathology, level II.
- 0752T: Digitization of glass microscope slides for surgical pathology, level III.
- 0753T: Digitization of glass microscope slides for surgical pathology, level IV.
- 0754T: Digitization of glass microscope slides for surgical pathology, level V.
- 0755T: Digitization of glass microscope slides for surgical pathology, level VI.
Category III Code Reimbursement
Medicare does not assign Relative Value Units (RVUs) to these digital pathology codes, so it does not pay for them. However, some commercial insurers reimburse these codes i.e.
- PPO, HMO, and indemnity plans with insurers like BCBS, AARP, UMR, Aetna, and Physicians Mutual can cover Category III Codes.
- Medicare and Medicaid managed care plans offered through UHC and similar companies may allow payment.
- Payments for Category III Code range from $20 to $35, if allowed.
Digital Pathology Workflow – How Digital Pathology Works?
Digital pathology has six (6) simple steps, from whole slide imaging to final diagnostic report generation.
1. Whole Slide Imaging – WSI
Whole Slide Imaging means the tissue slides are digitized to create high-resolution images for analysis and is the foundation of Digital pathology.
2. Workload Allocation
It is an essential stage in which all pathological cases are assigned to pathologists based on the type of diagnostic requirement. This step ensures optimum resource utilization and prioritization.
3. Use of WSI Viewer
Pathologists review WSI on a digital viewer that helps them diagnose sample tissue in high resolution.
Support Tools for Pathologists
- Routine Diagnostics: Pathologists conduct routine reviews using WSIs for diagnosis.
- Pre-Screening AI Tools: AI tools are used to handle cancer pre-screening. They help pathologists prioritize workload and reduce human intervention to the best possible level.
- Quantification Tools: Quantification tools assist pathologists in specific tasks, such as
- Mitosis Counting
- Tumour Grading
- Cancer Detection
- Immunohistochemistry Evaluation
4. WSI Annotation of Slides for Teaching Purpose
Pathologists mark the slides for educational purposes and ensure optimum utilization of information for future diagnostic purposes.
5. Composition of Report and Final Review
- Pathologists use speech-to-text tools to draft reports and streamline the documentation process.
- AI conducts a final review of the case before the report is signed off.
6. Written Report/Sign-Out
After completing the diagnostic procedures, the pathologist finalizes the report, which includes details of pathological procedures, tests, and results.
WSI Validation and Limitation
WSI has more promising results than traditional glass slides. In most studies, WSI has concordance rates greater than 95%. WSI’s limitations include its failure to identify microorganisms such as Helicobacter pylori, mitoses, and nuclear atypia.
The College of American Pathologists (CAP) and the Digital Pathology Association have set standards for professional organizations related to Digital pathology practices. These include;
- Standardized recommendations on equipment
- Pathology billing software
- Validation procedures to improve diagnostic outcomes.
Quality Parameters in WSI for Diagnostic Imaging
Implementation of Digital pathology requires sufficient handling of technical and operational aspects. Below, we have discussed four quality parameters that professionals must follow for diagnostic Digital imaging.
- Hardware and Ergonomics – High-definition screens and dedicated controllers simulating conventional microscopes allow pathologists to focus efficiently for a long time.
- Color Accuracy – Scanners and monitors are calibrated for precise color representation, which is a key parameter for differential diagnosis in digital pathology.
- Focus and Resolution – Single-plane scanning often misses details of microbes. Therefore, some techniques, such as z-stacking, can capture multiple focus levels, leading to a more substantial diagnosis.
- Artifact Management – It is an imperative quality parameter in WSI. In this issue, the image obscures details and needs to be minimized through proper scanning protocols and quality checks.
Regulatory Requirements for WSI for Patient Diagnostics in Europe and the U.S.
Patient safety and confidentiality of patients’ information are of great concern in Digital pathology. Regulatory bodies in Europe and the U.S. have established standards to guide the use of WSI in clinical diagnostics.
- European Union (EU) – WSI scanners are regulated under the In Vitro Diagnostic Directive (IVDD) and In Vitro Diagnostic Regulation (IVDR). These standards require performance evaluations and scientific validation for devices.
- United States (U.S.): The Food and Drug Administration (FDA) has approved selective WSI platforms for diagnostic use. The Philips IntelliSite Digital Pathology Solution and Sectra DP Module with Leica Scanner AT2 DX are examples of systems cleared after rigorous evaluation.
Compliance with these standards is imperative for laboratories. It ensures that Digital pathology systems are safe, accurate, and reliable for diagnostic use.
The Future trends in Digital Pathology
As Digital pathology continues to evolve, the following trends are shaping its future:
- AI Driven Pathology: Artificial intelligence is revolutionizing digital pathology through automated recognition of sample tissue, case prioritization, and predictive analytics. Multimodal AI integrates data from different pathology networks to improve patient diagnosis and treatment.
- Cloud Computing – it is the backbone of digital pathology as Cloud-based platforms provide scalable, secure storage and enable global collaboration in diagnostics and research, especially in underserved areas.
- Enhanced Diagnostics – High-resolution Digital imaging and AI analysis improve diagnostic accuracy, making pathology workflows faster and more reliable.
- Clinical Integration – Advanced image scanners and regulatory approvals boost the use of digital pathology in clinical settings. Automated reporting and workflow optimization are being facilitated by AI integration with digital pathology.
- Global Accessibility – Digital pathology provides remote consultations and collaborative research while maintaining high-quality care in even the most resource-constrained settings.
12th World Digital Pathology and AI UCG Congress
The 12th World Digital Pathology and AI UCG Congress will be held from December 17 to 19, 2024, at the Holiday Inn Dubai—Al Barsha in Dubai, UAE.
This hybrid conference will focus on integrating digital technology and Artificial intelligence in pathology. It will provide a platform for professionals to share knowledge, explore innovations, and discuss trends in the field.
The Takeaway!
Digital pathology is generally playing a crucial role in various ways. It transforms pathology services by converting standard glass slides into high-resolution WSI, which results in higher diagnostic accuracy and efficiency.
Secondly, its integration with Artificial intelligence tools can analyse complex patterns in tissue samples, thereby helping in the early detection of diseases. For example, AI can detect various cancers much more accurately than pathologists, improving the outcomes of diagnosis results.

Affan Sabir has an experience of more than a decade in providing revenue cycle management services to well reputed hospitals, labs & healthcare professionals.
A track record for helping clients improve their revenues drastically has made the author first choice for medical practitioners seeking to reduce their accounts receivables and get the best returns for their hard work from insurance companies.
